San Diego Brachial Plexus Injury Lawyer
Receive The Highest Compensation For Your Brachial Plexus Accident Case

Request a Free Legal Consultation
As Seen On


Our Accolades

HOW WE CAN HELP YOU IN YOUR BUS ACCIDENT CASE?
A brachial plexus is the nerve group that runs from the spine into your hands. The group has five nerves, each controlling a particular area and its capabilities. These start in the nerve roots in the neck (cervical) and shoulder (thoracic) areas of the spine and go through the arms. They are responsible for movement and sensation in these parts.
Brachial plexus injuries vary in their occurrence. They often occur as an injury in adulthood but are equally known as birth injuries. A brachial plexus injury can be mild or severe and cause minor issues or complete loss of use of the affected area. Medical malpractice and surgical errors can cause damage to these nerves, as can car accidents or contact sports.
If you experience difficulty with sensation or movement in your arm or shoulders following an accident, you should see a medical professional to see if you have a brachial plexus injury. Getting a doctor’s diagnosis is vital to get compensated for any potential losses your injury may cause. After a diagnosis, contact a personal injury lawyer from Mova Law Group, and we can help you file a claim. Contact us through this website or call us at (858) 900-9911 to set up a free case evaluation.


How Does a Brachial Plexus Injury Occur?
A brachial plexus injury occurs when the nerve bundle is pulled or compressed; this stress can sometimes result in a complete tearing of the nerves. The amount of pressure on the nerves will determine the severity of the injury.
Upper nerve Brachial plexus injuries happen when the neck and shoulders pull and push in opposite directions. Peripheral nerve injuries occur when one’s arm pulls above the shoulders (with force). Usually, brachial plexus injuries affect only one arm.

WHAT WE DO FOR OUR CLIENTS
- Maximum Compensation In Injury Law
- Medical Bills Paid
- Access To The Top Medical Professionals
- We Come To You In The Comfort Of Your Home
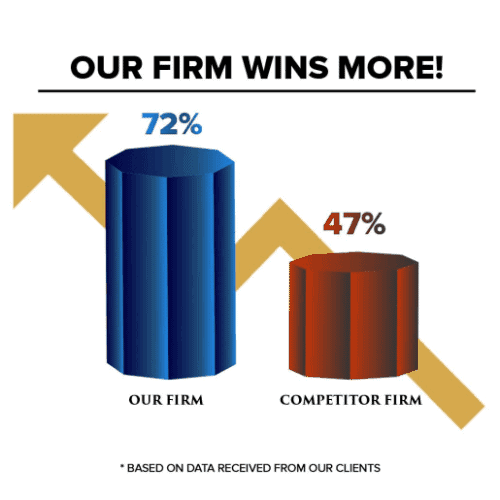
- Winning Track Record
- Transparency The Entire Process
- Property Damage Compensation
- Recovery Of Lost Wages
- Review Your Personal Injury Case
- Award-Winning Customer Service
- You Don’t Pay Unless We Win Your Case
Different Types of Brachial Plexus Injuries
Brachial plexus injuries vary in severity, and the nerve damage determines to which category an injury belongs.
Brachial Plexus Neuropraxia (Stretch)
- The most common brachial plexus injury is either compression or stretching of the nerves.
- Compression of the nerve root in the neck occurs more often in older adults.
- Traction neuropraxia involves stretching the nerves downwards. This type occurs most frequently in younger adults and adolescents.
- They are called “burners” or “stingers” in reference to the pain. You may experience flashes or a lingering sensation, or numbness. Discomfort may last less than a day or occur over a more extended period, depending on the severity of the injury.
- They are commonly caused by contact sports, particularly football or wrestling.
Brachial Plexus Rupture
- Results from the nerves being partially or fully ripped.
- Much more painful and severe than neuropraxia. You may experience movement difficulty or muscle weakness in the arm.

Brachial Plexus Neuroma
- Often referred to as a “pinched nerve.
- Scar tissue forms following an injury to the brachial plexus. This tissue forms knots and can cause pinching pain down your upper extremities, all in an attempt by the body to fix itself.
- Surgery may be necessary to fix this condition, and steps may be taken to prevent another neuroma. For example, the neurosurgeon may do a nerve graft to connect the damaged nerve to another.
Brachial Neuritis
- Often referred to as a “pinched nerve.
- Scar tissue forms following an injury to the brachial plexus. This tissue forms knots and can cause pinching pain down your upper extremities, all in an attempt by the body to fix itself.
- Surgery may be necessary to fix this condition, and steps may be taken to prevent another neuroma. For example, the neurosurgeon may do a nerve graft to connect the damaged nerve to another.
Brachial Neuritis
- Most severe brachial plexus injury. An avulsion occurs when the nerve root entirely severs from the spinal column.
- Avulsions are a result of physical trauma.
- No perfect fix for this injury and the effects will be permanent (weakness, sensation issues, possible paralysis)—surgery is often the only option for improvement.
Common Causes of Brachial Plexus Injuries
- Contact sports, especially wrestling, and football, for the potential compression or stretching. Athletes often feel “burners” and “stingers.”
- Birth injuries – Newborns can experience brachial plexus birth injuries. The likelihood of this injury depends on the labor’s complexity and the baby’s positioning. The baby’s shoulders can get stuck, causing stretching and compression. A healthcare provider may recklessly attempt to extract the baby through various means (forceps, vacuum) and cause damage to the baby’s upper nerves.
- Erb’s palsy is the most common brachial plexus birth injury, affects over 12,000 babies born yearly, and involves a weakness in the injured area. A baby can recover from this palsy and usually does within their first year of life (over 86% of pediatric patients).
- Brachial plexus palsy results in weakness in the shoulders, affecting the movement of the arm to meet the mouth for eating.
- Physical trauma includes car accidents, gunshot wounds, spinal cord injuries, and severe falls.
- Cancer – Tumors can grow on the brachial plexus network and cause compression, stretching, or harm. Treatment of the tumors by radiation can be just as harsh on the nerves.
If you or your child have experienced movement or sensation issues in your shoulders or arms, a San Diego personal injury attorney can help. If another person caused your injuries, they could be found liable, and our legal team can assist you in recouping some of your medical costs.
Symptoms of Brachial Plexus Injuries
You must seek medical attention for brachial plexus injuries to prevent permanent nerve damage. See a doctor if you experience one or more of the following:
- Recurring “burners” and “stingers,” or those lasting over time.
- Weakness in the arm or hand. It is imperative to see the doctor if both arms experience weakness.
- Neck pain.
A medical record of your injuries helps build your personal injury case in the aftermath of an accident. Our team of personal injury lawyers can also connect you with top medical professionals if needed.
Doctors can diagnose brachial plexus injuries in a few different ways:
- X-rays help rule out broken bones as the root cause of your pain. X-rays can also highlight possible lung damage resulting from damaged nerves in this organ.
- A CT scan or MRI can identify avulsions.
- Electromyography (EMG) looks at muscle and nerve functioning. These tests help establish a baseline for your muscles and identify the problems.

What Our Experienced Brachial Plexus Injury Attorneys Will Do For You
- We Will Ensure Your Personal Health Is Taken Care Of.
- We Will Ensure Your Damages Are Reimbursed For Free.
- We Will Connect You With Top Rated Doctors For Treatment.
Brachial plexus injuries come at a cost, but you shouldn’t be fighting the insurance companies for something that was not your fault!
Brachial Plexus Injury Recovery and Complications
Usually, the best treatment for these injuries is time. Most birth injuries resolve themselves, and neuropraxia in adults needs some time for the nerve to heal itself.
More severe injuries can cause pain and potential disability. The following conditions are a result of brachial plexus injuries:
Chronic pain from nerve damage.
Lasting numbness increases the risk of hurting yourself without realizing it.
Stiffness in joints due to temporary paralysis. Moving can remain challenging, even after recovery.
Muscle atrophy, as damaged nerves cannot communicate appropriately with muscles. Constant weakness can also cause muscle atrophy since you can’t use them.
Permanent disability – As a result of the initial incident or improper healing. There are some severe injuries from which you can never fully recover.
Brachial Plexus Injury Treatment
The preferred treatment method for brachial plexus injuries is time. Still, you may have to consider other options if waiting will hinder recovery. It’s natural to want to avoid surgery, especially if a surgical error or medical malpractice caused the initial injury. However, it may be your best option, so consult a doctor for suggestions.
An expert brachial plexus injury lawyer may recommend the following:
- Physical Therapy – Exercises improving the range of motion and flexibility in stiff muscles and joints may be a part of physical therapy to restore arm and hand function.
- Corticosteroid Creams or Injections – For pain management and quicker healing.
- Assistive Devices – A brace, a splint, or compression sleeves can help speed recovery.
- Medication – Pain management.
- Occupational Therapist – Patients with severe muscle weakness, numbness, and pain will need occupational therapy to re-learn practical skills such as dressing and cooking.

Brachial Plexus Surgical Options
In cases where the injuries to the brachial plexus fail to heal on their own, they may require surgery to repair the damage. Brachial plexus surgery produces results gradually, so it may take months or years for patients to see a noticeable change.
To optimize nerve recovery, it is best to have brachial plexus surgery within six months of an injury. You may need to decide between surgery and taking time to recover naturally. Your neurosurgeon might prescribe the following reconstructive procedures:
- Nerve Repair – Putting a torn nerve back together.
- Neurolysis – To improve the function of the injured nerve, the neurosurgeon slashes the nerves to remove scar tissue.
- Nerve Grafts – A nerve graft is another way to treat severe brachial plexus injuries. Nerve grafting connects the ends of a damaged nerve with a healthy nerve from another area of the body to guide the healing process.
- Nerve Transfers – The nerve transfer process attaches a less critical but still functional nerve to a damaged nerve, thus creating a framework for new nerve growth.
- Tendon & Muscle Transfer – The surgeon may transfer a tendon or muscle from one part of the body to another to restore normal function.
Consult your healthcare provider for help deciding whether surgery is right for you. For newborns with birth injuries or individuals with neurological challenges, it may be best to allow time to resolve your injuries and avoid further damage. Mova Law Group’s experienced personal injury lawyers will review your medical records and accident evidence with you and provide you with your legal options.

How Can I Prevent an Injury to the Brachial Plexus?
Several things can help prevent an injury to the brachial plexus, including:
- Wearing seatbelts while in motor vehicles.
- Using the appropriate safety equipment while playing sports.
- Using the proper safety equipment when working around machinery.
- Exercising caution during any activity that could cause harm.
It is essential to be aware of the risks involved in any activity and to take precautions to avoid injuries. Learning proper stretches before playing sports can help prevent injuries. Wearing the right protective gear while playing sports or working at a hazardous job site can also help avoid accidents.
A San Diego Brachial Plexus Injury Lawyer Helps You Recover Damages
The results of a brachial plexus injury are sometimes far-reaching in your life. Costs add up for more severe and long-term injuries, and you can risk bankruptcy. A personal injury attorney from San Diego‘s top-rated Mova Law Group can examine the evidence from your case. We will help determine whether you have a liable case against a doctor or other individual responsible for your pain.
Experienced injury lawyers can estimate the economic and non-economic costs of your injury. These costs may include the following:
- Medical bills (past and future).
- Decreased or lost wages (including into the future).
- Pain and suffering.
- Occupational therapy.
- Pain and suffering.
- Loss of quality and enjoyment of life.
Our initial case evaluation is of no charge to you so that you can discuss your case with no obligation. We will work with you on a contingency fee plan if we take your injury case. You will only pay once we get your maximum compensation. Our top-rated brachial plexus injury attorneys will advance your personal injury claim and handle negotiations. At the same time, you focus on the important business of recovery. Contact us today to set up your free consultation at (858) 900-9911 or through this website.

Chris Mova is an award-winning brachial plexus injury lawyer in San Diego, California. His law firm of Mova Law Group fights for you against the big insurance companies. Chris knows the value of listening to each client’s unique experience, and his team of personal injury attorneys was hand-picked because they feel the same way. He is committed to getting you justice and fair treatment when you need it most. Learn more about Chris.